Definition
Transfusion is the process of transferring whole blood or blood components from a donor to a recipient.
Purpose
Transfusions are given to restore lost blood, to improve clotting time, and to improve the ability of the blood to deliver oxygen to the body's tissues. About 32,000 pints of donated blood are transfused each day in the Nigeria.
The three main reasons why a child may need a blood transfusion are:
Loss of blood during surgery or from an injury or an illness.An inability to make enough blood.Some illnesses and treatments can harm the bone marrow's ability to make blood (e.g., chemotherapydecreases production of new blood cells).To prevent complications from an existing blood or bleeding disorder, such as sickle cell disease, thalassemia, or anemia caused bykidney disease, hemophilia, or von Willebrand disease.
Where the Blood Comes From
Because there's no manmade substitute for blood, the blood supply used for transfusion must be donated. The three types of blood donation are:
Autologous (ah-TOL-uh-gus) blood donation. Sometimes, when people know in advance that they are going to need a transfusion (for a planned surgery, for example), they may donate their own blood beforehand. There's no age requirement, but in general, kids don't donate their blood for their own use until they're over age 12.
Directed donation. This is when a family member or friend with a compatible blood type donates blood specifically for use by a designated patient.
Volunteer donation. Since there's no medical evidence that blood from directed donors is any safer than blood from volunteer donors, most patients receive blood donated through blood drives, which are often run by independent collection agencies like the American Red Cross. The minimum age for donating blood is 16 or 17 years old, depending on where a person lives.
Some people worry about getting diseases from infected blood, but the United States has one of the safest blood supplies in the world. Many organizations, including community blood banks and the federal government, work hard to make sure that the blood supply is safe.
The risk of getting a disease like HIV or hepatitis through a transfusion is extremely low in the Nigeria today because of very stringent blood screening. Also, the needles and other equipment used are sterile, and are used only on one person and then thrown away in special containers.
Description
Blood is collected from the donor by inserting a large needle into a vein in the arm, usually one of the larger veins near the inside of the elbow. A tourniquet is placed on the upper arm to increase the pressure in the arm veins, which makes them swell and become more accessible. Once the nurse or technician has identified a suitable vein, she or he sterilizes the area where the needle will be inserted by scrubbing the skin with a soap solution or an antiseptic that contains iodine. Sometimes both solutions are used. The donor lies on a bed or cot during the procedure, which usually takes between 10 and 20 minutes. Generally, an 18-gauge needle is used. This size of needle fits easily into the veins and yet is large enough to allow blood to flow easily. Human blood will sometimes clot in a smaller needle and stop flowing. The donor's blood is collected in a sterile plastic bag that holds one pint (450 ml). The bags contain an anticoagulant to prevent clotting and preservatives to keep the blood cells alive. A sample of the donator's blood is collected at the time of donation and tested for infectious diseases. The blood is not used until the test results confirm that it is safe. Properly handled and refrigerated, whole blood can last for 42 days.
The recipient of a transfusion is prepared in much the same way as the blood donor. The site for the needle insertion is carefully washed with a soap-based solution followed by an antiseptic containing iodine. The skin is then dried and the transfusion needle inserted into the vein. During the early stages of a transfusion, the recipient is monitored closely to detect any adverse reactions. If no signs of adverse reaction are evident, the patient is monitored occasionally for the duration of the transfusion period. Upon completion of the transfusion, a compress is placed over the needle insertion site to prevent extensive bleeding.
Blood typing
All donated blood is typed, which means that it is analyzed to determine which of several major and minor blood types (also called blood groups) it belongs to. Blood types are genetically determined. The major types are classified by the ABO system. This system groups blood with reference to two substances in the red blood cells called antigen A and antigen B. The four ABO blood types are A, B, AB, and O. Type A blood has the A antigen, type B has the B antigen, type AB has both, and type O has neither. These four types of blood are further classified by the Rh factor. The Rh, or rhesus factor, is also an antigen in the red blood cells. A person who has the Rh factor is Rh positive; a person who does not have the factor is Rh negative. If a person has red blood cells with both the B and the Rh antigens, that person is said to have a B positive (B+) blood type. Blood types determine which kinds of donated blood a patient can receive. Generally, patients are limited to receiving only blood of the exact same ABO and Rh type as their own. For example, a person with B+ blood can receive blood or blood cells only from another person with B+ blood. An exception is blood type O. Individuals with type O blood are called universal donors, because people of all blood types can accept their blood.
Blood can also be typed with reference to several other minor antigens, such as Kell, Kidd, Duffy, and Lewis. These minor antigens can become important when a patient has received many transfusions. These patients tend to build up an immune response to the minor blood groups that do not match their own. They may have an adverse reaction upon receiving a transfusion with a mismatched minor blood group. A third group of antigens that may cause a reaction are residues from the donor's plasma attached to the RBCs. To eliminate this problem, the RBCs are rinsed to remove plasma residues. These rinsed cells are called washed RBCs.
Other transfusion procedures
Autologous transfusion is a procedure in which patients donate blood for their own use. Patients who are to undergo surgical procedures requiring a blood transfusion may choose to donate several units of blood ahead of time. The blood is stored at the hospital for the patient's exclusive use. Autologous donation assures that the blood type is an exact match. It also assures that no infection will be transmitted through the blood transfusion. Autologous donation accounts for 5% of blood use in the United States each year.
Directed donors are family or friends of the patient who needs a transfusion. Some people think that family and friends provide a safer source of blood than the general blood supply. Studies do not show that directed donor blood is any safer. Blood that is not used for the identified patient becomes part of the general blood supply.
Apheresis is a special procedure in which only certain specific components of a donor's blood are collected. The remaining blood fractions are returned to the donor. A special blood-processing instrument is used in apheresis. It fractionates the blood, saves the desired component, and pumps all the other components back into the donor. Because donors give only part of their blood, they can donate more frequently. For example, people can give almost ten times as many platelets by apheresis as they could give by donating whole blood. The donation process takes about one to two hours.
Preparation
The first step in blood donation is the taking of the donor's medical history. Blood donors are questioned about their general health, their lifestyle, and any medical conditions that might disqualify them. These conditions include hepatitis, AIDS, cancer, heart disease, asthma, malaria, bleeding disorders, and high blood pressure. Screening prevents people from donating who might transmit diseases or whose medical condition would place them at risk if they donated blood. Some geographical areas or communities have a high rate of hepatitis or AIDS. Blood collection in most of these areas has been discontinued indefinitely.
The blood pressure, temperature, and pulse of donors are taken to ensure that they are physically able to donate blood. One pint (450 mL) of blood is usually withdrawn, although it is possible to donate smaller amounts. The average adult male has 10–12 pints of blood in his body; the average adult female has 8–9 pints in hers. Within hours after donating, most people's bodies have replaced the fluid lost with the donated blood, which brings their blood volume back to normal. Replacement of the blood cells and platelets, however, can take several weeks. Pregnant women and people with low blood pressure or anemia should not donate blood or should limit the amount of blood they give. Generally, people are allowed to donate blood only once every two months. This restriction ensures the health of the donor and discourages people from selling their blood. The former practice of paying donors for blood has essentially stopped. Donors who sell blood tend to be at high risk for the transmission of bloodborne diseases.
Aftercare
Recipients of blood transfusion are monitored during and after the transfusion for signs of an adverse reaction. Blood donors are generally given fluids and light refreshments to prevent such possible side effects as dizziness and nausea. They are also asked to remain in the donation area for 15–20 minutes after giving blood to make sure that they are not likely to faint when they leave.
Risks
Risks for donors
For donors, the process of giving blood is very safe. Only sterile equipment is used and there is no chance of catching an infection from the equipment. There is a slight chance of infection at the puncture site if the skin is not properly washed before the collection needle is inserted. Some donors feel lightheaded when they sit up or stand for the first time after donating. Occasionally, a donor will faint. Donors are encouraged to drink plenty of liquids to replace the fluid lost with the donated blood. It is important to maintain the fluid volume of the blood so that the blood pressure will remain stable. Strenuous exerciseshould be avoided for the rest of the day. It is normal to feel some soreness or to find a small bluish bruise at the site of the needle insertion. Most donors have very slight symptoms or no symptoms at all after giving blood.
Risks for recipients
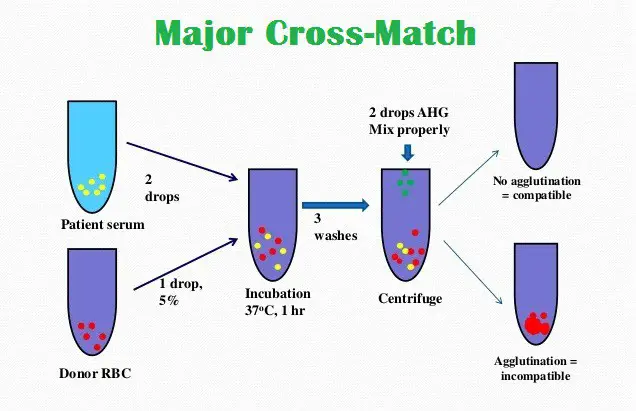
A number of precautions must be taken for transfusion recipients. Donated blood must be matched with the recipient's blood type, as incompatible blood types can cause a serious adverse reaction (transfusion reaction). Blood is introduced slowly by gravity flow directly into the veins (intravenous infusion) so that medical personnel can observe the patient for signs of adverse reactions. People who have received many transfusions may develop an immune response to some factors in foreign blood cells (see below). This immune reaction must be evaluated before the patient is given new blood.
Adverse reactions to mismatched blood (transfusion reaction) is a major risk of blood transfusion. Transfusion reaction occurs when antibodies in the recipient's blood react to foreign blood cells introduced by the transfusion. The antibodies bind to the foreign cells and destroy them. This destruction is called a hemolytic reaction. In addition, a transfusion reaction may also cause a hypersensitivity of the immune system that may in turn result in tissue damage within the patient's body. The patient may also have an allergic reaction to mismatched blood.
The first symptoms of transfusion reaction are a feeling of general discomfort and anxiety. Breathing difficulties, flushing, and a sense of pressure in the chest or back pain may also be present. Evidence of a hemolytic reaction can be seen in the urine, which will be colored from the hemoglobinleaking from the destroyed red blood cells. Severe hemolytic reactions are occasionally fatal. Reactions to mismatches of minor factors are milder. These symptoms include itchiness, dizziness, fever, headache, rash, and swelling. Sometimes the patient will experience breathing difficulties and muscle spasms. Most adverse reactions from mismatched blood are not life-threatening.
Infectious diseases can also be transmitted through donated blood and constitute another major risk of blood transfusion. The infectious diseases most often acquired from blood transfusion in the United States are hepatitis and HIV.
Patients who are given too much blood can develop high blood pressure, a concern for people who have heart disease. Very rarely, an air embolism is created when air is introduced into a patient's veins through the tubing used for intravenous infusion. The danger of embolism is greatest when infusion is begun or ended. Care must be taken to ensure that all air is bled out of the tubing before infusion begins, and that the infusion is stopped before air can enter the patient's blood system.
Normal results
Most individuals will feel only a slight sting from the needle used during the blood donation process, and will not experience any side effects after the procedure is over. Plasma is regenerated by the body within 24 hours, and red blood cells within a few weeks. Patients who receive a blood transfusion will usually experience mild or no side effects.
Morbidity and mortality rates
The risk of acquiring an infectious disease from a blood transfusion is very low. The risk of HIV transmission is one in 450,000 to 660,000 units of blood; hepatitis B virus (HBV), one in 137,000 units; and hepatitis C virus (HCV), one in 1,000,000 units. Bacterial contamination (a cause of infection) is identified in one in 4,200 transfusions. Approximately one in 25,000 individuals who receive a blood transfusion will develop a hemolytic reaction; the risk of a fatal hemolytic reaction is one in 160,000.
Alternatives
There are several alternatives to blood transfusion as of 2003. These include:
Volume expanders. Certain fluids (saline, Ringer's lactate solution, dextran, etc.) may be used to increase the patient's blood volume without adding additional blood cells.Blood substitutes. Much research is currently being done into compounds that can replace some or all of the functions of blood components. One such compound, called HBOC-201 or Hemopure, is hemoglobin derived from bovine (cow) blood. Hemopure shows promise as a substitute for red blood cell transfusion.Bloodless surgery. It may be possible to avoid excessive blood loss through careful planning prior to surgery. Specialized instruments can minimize the amount of blood lost during a procedure. It is also possible to collect some of the blood lost during surgery and reinfuse it into the patient at the end of the operation.