Diabetes mellitus is a condition that results when the pancreas produces little or no insulin, or when the cells of the body cannot use the insulin produced effectively. When insulin is absent or ineffective, the cells of the body cannot absorb glucose (sugar) from blood to provide the body with energy.
KEYWORDS
for searching the Internet and other reference sources
Carbohydrate metabolism
Insulin resistance
Polyuria
Melinda's Story
Melinda had just turned twelve and felt hungry all the time. Her stomach growled in class and her after-school snack no longer held her until dinner. No matter how many trips she made to the school water fountain, she was always thirsty. Even worse, she could not believe how often she needed to go to the bathroom. One of her teachers, after signing Melinda's seventh bathroom pass for the day, suggested that Melinda ask her parents to take her to the doctor. She thought that Melinda might have diabetes, and she was right.
What Is Diabetes?
Diabetes is a group of related diseases characterized by elevated levels of glucose (sugar) in the blood. It is caused by the failure of the pancreas to produce sufficient insulin, or any insulin at all. It can also be caused by the failure of the body's cells to make proper use of the insulin that is produced.
* hormones are chemicals that are produced by different glands in the body. Hormones are like the body's ambassadors: they are created in one place but are sent through the body to have specific regulatory effects in different places.
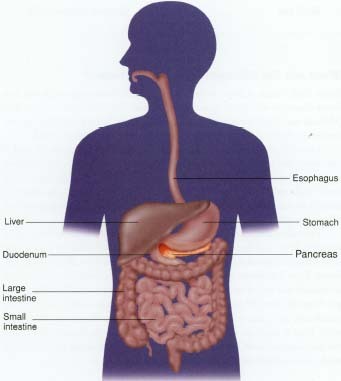
The pancreas, the site of insulin production, is a large gland near the stomach. It contains groups of cells that function like tiny factories, producing different hormones * at exactly the right time and in the right amount. These groups (or "islands") of cells are called islet (EYE-let) cells.
One type of islet cell is called a beta (BAY-ta) cell. Beta cells are responsible for producing a hormone called insulin. The human body needs insulin to function, because insulin helps the body use food for energy.
When people eat, their bodies break food down and convert it into sugars and other fuels. The main fuel is a sugar called glucose (GLOO-kose). When it is in the blood, it is called "blood glucose" or sometimes "blood sugar." Glucose provides the energy people need to carry out almost every task, from pumping blood to walking to reading a book. But glucose cannot get too far on its own—insulin must be there to allow it to pass into the body's cells.
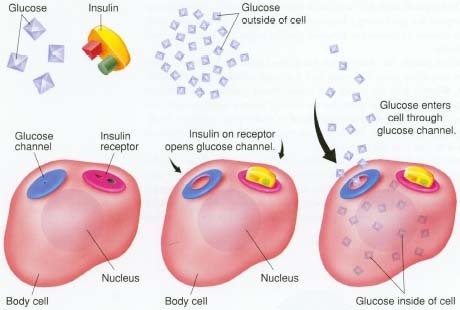
Insulin works like a key, "unlocking" the door to cells. When insulin production stops or slows down in the beta cell factory, the body's cells cannot take in the glucose they need for energy. People with diabetes get glucose from their food, but no matter how much they eat, if the insulin "key" is absent or not working properly, their glucose fuel is "locked out" of the body's cells.
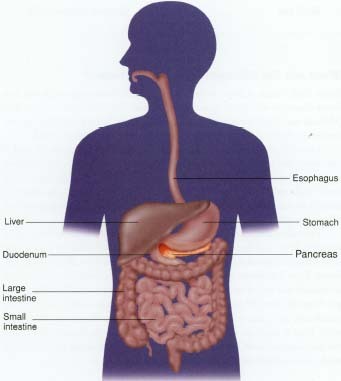
The pancreas is one of the most important organs in the body. It has several functions as part of the endocrine (hormone-producing) system and the digestive system.
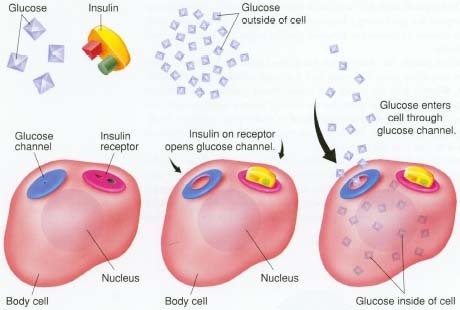
The hormone insulin is the key that unlocks the body cell's glucose channel, allowing glucose ("blood sugar") to enter the cell and refuel it. Without the insulin key, glucose is locked out of the cell and must remain in the bloodstream.
What Are the Different Types of Diabetes?
More than fifteen million people in the United States have diabetes, but fewer than one million of those people (about 750,000) have the type that Melinda has. This type is known as Type 1 diabetes. It is also called immune-mediated diabetes or insulin-dependent diabetes mellitus (IDDM).
Type 1 diabetes is usually diagnosed before a person turns 19, and is therefore also referred to as "juvenile" diabetes. About 125,000 children and teenagers in the United States today have Type 1 diabetes. They make little or no insulin of their own, so they depend on injections of insulin to stay healthy. They also need to make lifestyle changes, such as when and what they eat.
The other fourteen-plus million Americans with diabetes have what is called Type 2 diabetes. Other names for this kind of diabetes include
non-insulin-dependent diabetes mellitus (NIDDM) or adult-onset diabetes. Type 2 diabetes occurs when the cells of the body do not respond to insulin the way they should. This type of diabetes usually affects people who are over 40 years old. Extra body fat often contributes to this condition and, many times, weight loss can help remedy it. A person with Type 2 diabetes is not necessarily dependent on insulin injections the way a person with Type 1 diabetes is. Type 2 diabetes can also be treated with pills in addition to a change in diet.
What Causes the Different Types of Diabetes?
Type 1 diabetes
Type 1 diabetes is not contagious like a cold or chickenpox: people cannot catch it from one another. Nor do people get Type 1 diabetes suddenly. It usually takes months or years to develop in a person's body. Despite what many people think, Type 1 diabetes isn't caused by eating too many sweets.
Although scientists do not know exactly what causes Type 1 diabetes, they have enough evidence to suggest that there are at least a couple of different reasons why one person might develop it while another would not: genes and environmental triggers.
- Genes. People with Type 1 diabetes are born with certain genes for the illness, just as they are born with genes for blue eyes or brown eyes. Genes are something people inherit from their parents before they are born. In some families, the genes for Type 1 diabetes are passed from parents to more than one child; a sibling of someone with Type 1 diabetes has about a 5 percent chance of also developing it.
- Environmental triggers. Some people have Type 1 diabetes set in motion by an environmental trigger, like a virus. The trigger will make the person's immune system attack and destroy the beta cells, with the result that insulin can no longer be produced. However, for an environmental trigger to have this effect, people probably have to have a genetic predisposition to it. Most people do not just suddenly develop diabetes because they get the flu.
Type 2 diabetes
Just as with Type 1 diabetes, people with Type 2 diabetes are not contagious. Two major factors seem to play a role in why people develop Type 2 diabetes: genes and obesity (or being overweight).
- Genes. Just as certain genes may mean that a person may be more likely to develop Type 1 diabetes, other genes play an important part in people who develop Type 2 diabetes.
- Obesity. Many people who have Type 2 diabetes are obese. Scientists think that this extra weight may impair the body's ability to use insulin effectively.
How Do People Know If They Have Diabetes?
Symptoms
When the body does not have adequate amounts of insulin, symptoms like Melinda's result.
Frequent urination is very common in a person with Type 1 diabetes. This happens because glucose cannot get into the body's cells and builds up in the blood instead. Normally, the kidneys do not allow glucose to get into the urine. But in the case of diabetes, the high level of blood glucose spills into the urine, pulling extra water out of the body along with it.
Feeling very thirsty is also common, because the body needs to make up for all the liquid lost through urination. Feeling hungry and eating a lot are also common symptoms; the body is looking for a way to get the energy that it is missing. But even with all the extra eating, people with undiagnosed diabetes may lose weight, because their bodies start to use fat for energy instead of sugar. In the case of growing children and teenagers, the fact that they are not gaining weight at a time in their lives when they should be may be a sign that diabetes may be present.
These symptoms are common to both Type 1 and Type 2 diabetes, although usually less severe in the latter. Type 2 diabetes may sometimes present with other symptoms, such as repeated or hard-to-heal infections, blurred vision, and dry, itchy skin. But often these symptoms are quite mild, and due attention is not paid to them.
Diagnosis
If a doctor suspects that a patient has diabetes, usually he or she will first do a urine test. The test is simple: it involves a small sample of the patient's urine and special strips of paper that are treated with a chemical to detect glucose. If the immersed strip shows that glucose is present, the doctor will want to confirm the test by checking the patient's blood sugar with a blood test. If the doctor feels sure that there is too much glucose in the patient's blood, further evaluation and testing will be done, and treatment will be started if the diagnosis of diabetes is confirmed.
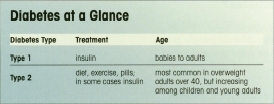
Diabetes at a Glance
| Diabetes Type | Treatment | Age |
| Type 1 | insulin | babies to adults |
| Type 2 | diet, exercise, pills;
in some cases insulin | most common in overweight
adults over 40, but increasing
among children and young adults |
Two Millennia of Medicine
The ancient Greek physician Aretaeus (ar-e-TE-us) of Cappadocia (c. 81—c. 138) described diabetes as a "melting down of the flesh and limbs into urine." Throughout history, many people with the disease died at an early age by wasting away, although the disease was probably not as prevalent in ancient times as it is now.
Treatments frequently involved dietary changes. Aretaeus recommended milks, cereals, and starches. In 1797, John Rollo recommended a meat diet high in proteins. These diets were not cures for diabetes, but they did allow people with diabetes to live longer than if they had remained on standard diets.
The first truly successful treatment for diabetes was finally made available in the 1920s when
Frederick Banting, Charles Best, and John James Macleod first isolated insulin for use through therapeutic injections.
Because people with Type 2 diabetes continue to make insulin that is functioning to a certain extent, they may develop symptoms over a period of months or years without facing immediate danger. They may feel tired, worn out, or thirsty much of the time, without thinking that it could be diabetes. In many cases, Type 2 diabetes is actually discovered by accident, during a routine physical exam or screening blood or urine test.
How Is Type 1 Diabetes Treated?
A person who has been diagnosed with Type 1 diabetes needs to do a number of things to function well. These include taking insulin, following a food plan, exercising, monitoring blood glucose levels, and taking urine tests. All of these things contribute toward achieving the major goal: keeping the amount of glucose in the blood as close to normal as possible, so the person with diabetes stays healthy and feels good, now and in the future.
Insulin
People with Type 1 diabetes must get the correct amount of insulin into their blood. Different sources of insulin have been used to treat diabetes. Pork insulin is extracted from the pancreas of a pig, but human insulin does not come from the pancreas of a human. Instead, human insulin is synthetic. It is made in a laboratory, and is the type most commonly used to treat diabetes today.
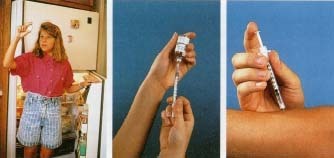
Insulin comes in liquid form (dissolved in water) in a bottle and must be injected into the body. Unlike a lot of medications, insulin cannot be swallowed in pill form because the hormone insulin is a protein. Like other proteins, it would be digested and broken apart in the stomach, just like the protein contained in food.
Most people take insulin by using a needle to inject it into the layer of fat beneath the skin. The most common places where people take insulin are in their arms, legs, stomach, and hips—all places where people have some fat. The injection does not hurt very much, since the needle is very thin. Usually, a person needs to inject insulin this way two or more times a day, on a set schedule, coordinated with meals.
Some people with Type 1 diabetes use an insulin pump. It is about the same size as a beeper, with a small container filled with insulin. The insulin gets automatically "pumped" into the person's body through a small tube attached to a needle inserted into the skin. The insulin is pumped in at a slow rate all the time, with an extra "boost" pumped in before meals to prepare the body for the incoming sugar.
However people with Type 1 diabetes take insulin, one thing stays constant: they must take insulin every single day to allow the body's cells to take in and use glucose properly. They cannot take a break or decide to stop taking it, or they will become ill.
Sports Stars with Type 1
Diabetes
These outstanding athletes were all diagnosed with Type 1 diabetes at an early age:
- Jackie Robinson Robinson was the baseball immortal who broke the color barrier in 1947. In his 10-year career with the Brooklyn Dodgers, Robinson was a batting champion, the League MVP, and a member of six championship teams. He was elected to the Hall of Fame in 1962, his first year of eligibility.
- Bobby Clarke The tenacious leader of hockey's Philadelphia Flyers for 15 seasons, Bobby Clarke was first diagnosed with diabetes at the age of 15. Undeterred, he went on to win three Hart Trophies as league MVR
- Wade Wilson An NFL quarterback for over 16 years, beginning in 1981, Wilson led the Minnesota Vikings to three playoffs and the 1987 NFC Championship game.
Food
Proper nutrition is a very important part of staying healthy—for everyone—and especially for a person with Type 1 diabetes. Since food affects how much glucose is in the blood, people with Type 1 diabetes must pay careful attention to the food they eat, how much they eat, and when they eat it. In particular, since carbohydrates are the body's main source of glucose, many people with diabetes estimate the amount of carbohydrates in each meal to determine if they are getting the right amount of sugar.
All that does not mean that the eating habits of someone with diabetes are so very different from other people. The food itself can be the same as that eaten by most people. But in most cases, their meal plans must be on some sort of schedule, include snacks, and limit sweets because of the large amount of sugar they contain.
Exercise
Just like healthy eating, exercise is something that is important for everyone and especially for people with Type 1 diabetes. It was not too long ago that some doctors thought people with Type 1 diabetes should not exercise, but that opinion has changed. Exercise helps insulin work better to control the level of glucose in the blood. Exercise also helps keep people with diabetes at the right weight, and it helps maintain a healthy heart and blood vessels. In addition, exercise helps people feel good about themselves.
When people with Type 1 diabetes exercise, they use glucose at a faster-than-normal rate, so they must pay special attention to ensure that their blood glucose level does not drop too low. This may mean taking less insulin, eating more before exercise, or having snacks during and after exercise.
Blood glucose and urine testing
People who have Type 1 diabetes usually test their blood glucose three or more times a day. This involves pricking the finger with a tiny, sharp device to get a drop of blood. The blood drop is put on a chemical strip and inserted into a testing meter that "reads" the amount of sugar in the blood. The person then records the blood glucose numbers in a diary. This monitoring helps to determine if the level of glucose in the blood is where it should be and guides adjustment in the treatment plan.
Urine testing is another helpful form of monitoring. It is especially important when a person with Type 1 diabetes is sick (with the flu, for example). Any kind of physical stress, such as an infection, tends to interfere with the body's cells taking in and using glucose properly. When this happens, the cells begin to break down fat for energy. A potentially harmful byproduct of this process is the production of ketones * . Urine testing is an effective means of determining if ketones are building up in the blood.
Hypoglycemia, Hyperglycemia, and Ketoacidosis
Sometimes, even with insulin, proper nutrition, and exercise, it can be difficult to control diabetes completely. Blood glucose levels can become either too high or too low in some cases, and blood levels of ketones can rise to toxic levels.
* ketones (KEE-tones) are the chemicals produced when the body breaks down fat for energy. In large amounts, ketones are poisonous; as they build up in the blood, they become increasingly toxic.
Hypoglycemia
If the level of glucose in the blood is too low, this is called
hypoglycemia (hy-po-gly-SEE-mee-a). This can result when someone takes too much insulin, misses a meal or snack, or exercises too hard without taking special precautions. In its beginning stages, hypoglycemia can make someone weak, shaky, dizzy, and sweaty. A person with diabetes learns to be very aware of these warning signs and almost always takes action
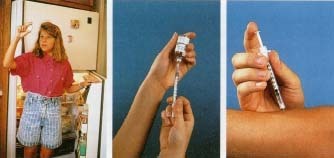
A girl with diabetes removes a vial of insulin from the refrigerator (left). The insulin is drawn out of the bottle with a small insulin syringe (center). The needle is thin and lubricated, so it hardly hurts at all when it goes in (right).
to treat them, by drinking some juice or taking glucose tablets, before they become severe. If left untreated, a person may become disoriented, sleepy, or have a hard time talking. Eventually, he may become very confused and uncoordinated and, in extreme cases, go into a coma * . The treatment for an extreme case of hypoglycemia is to give the person sugar as soon as possible, by intravenous * injection if necessary.
Hyperglycemia
Another problem that people with Type 1 diabetes can have is too much glucose in the blood, called
hyperglycemia (hy-per-gly-SEE-mee-a). When there is too much sugar in the blood, it is often because the person has taken too little insulin, has eaten too
much high-sugar food, or is ill with an infection or stressed for other reasons. Symptoms include very frequent urination, extreme thirst, weakness, and tiredness.
Ketoacidosis
In uncontrolled diabetes, when the blood becomes too acidic because of high levels of ketones in it, the condition that results is called ketoacidosis (ke-to-a-si-DO-sis). A person in ketoacidosis may be nauseated or vomiting and breathing very deeply. If he does not get treatment, he will become dehydrated and go into a coma. Emergency treatment involves insulin and lots of fluids, usually by intravenous injection. Fortunately, ketoacidosis is almost always preventable in people whose diabetes has been diagnosed, and who take care to manage their diabetes properly.
How Is Type 2 Diabetes Treated?
People who have Type 2 diabetes are often able to treat their diabetes with dietary changes and a weight-control program, if needed. This consists of balancing a healthy combination of foods and exercise.
In some cases, people with Type 2 diabetes are treated with pills. These pills do not contain insulin, but they help the body to make more insulin or respond to insulin more normally. Sometimes, a person with Type 2 diabetes will need to take insulin injections, like a person with Type 1 diabetes.
* coma is an unconscious state, like a very deep sleep. A person in a coma cannot be awakened, and cannot move, see, speak, or hear.
* intravenous (in-tra-VEE-nus) means injected directly into the veins
Diabetes Research
Clinical trials are research projects undertaken by scientists, pharmaceutical companies, and government researchers to investigate whether medications and treatment plans are safe and effective.
To evaluate the effectiveness of careful self-management in reducing the long-term complications of diabetes, in 1983 the U.S. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) undertook a large ten-year study, called the Diabetes Control and Complications Trial (DCCT for short).
People with diabetes took part in the DCCT and followed instructions for testing their blood glucose three or four times a day, taking more frequent insulin injections or using an insulin pump, and following a healthy meal plan. The test results showed that the people who maintained near-normal blood glucose levels had fewer long-term complications, such as problems with their hearts, eyes, or kidneys. It proved that for a person with diabetes, paying close attention to small things on a daily basis has a big payoff later on.
There are many similarities in the treatments for Type 1 and Type 2 diabetes, but the main difference is the role of insulin. If a person with Type 2 diabetes forgets to take his insulin, he will not go into ketoacidosis. And while a doctor might say it is all right for a person with Type 2 diabetes to stop taking insulin completely and just take pills, this would not be possible for a person with Type 1 diabetes.
What Is It Like to Live With Type 1 or Type 2 Diabetes?
Between taking insulin, following a meal plan, testing blood sugar levels, and the rest, living with Type 1 diabetes can sound like a big job—and it can be—especially in the beginning. Luckily, many people who have been diagnosed with Type 1 diabetes have an entire diabetes treatment team to help them along. This team usually includes a doctor, a diabetes nurse, a dietician, a psychologist, and a social worker. Ideally, the entire team works to become partners with the patient and the patient's family, so that they can maintain as normal a life as possible.
People with diabetes can do almost everything that people without diabetes can. They can:
- go to school
- play sports
- spend time with friends
- eat food at parties
- do almost every kind of job
- go to college
- get married
A person with diabetes may have to eat an extra snack before competing in a track meet, or duck out of a party for a minute to take insulin, or have only a small bit of ice cream when everyone else is going for the Super Sundae. But people who control their diabetes lead normal lives. And women with diabetes who want to have babies can usually do so, with the support of their diabetes treatment team.
The U.S. and the World
Globally, there were approximately 135 million adults with diabetes in 1995. By the year 2025, that number is expected to rise to 300 million.
- By the year 2025, it is estimated that the number of persons with diabetes will be over 57 million in India, 37 million in China, and 22 million in the United States.
- In 1997, there were more than 15 million people with diabetes in the U.S. Of those, more than 5 million had not been diagnosed.
- Over 90 percent of diabetes cases are Type 2 diabetes. While Type 1 (the type that affects most children and teenagers with diabetes) is most common in Americans of European descent, the prevalence of Type 2 diabetes is 2 to 4 times higher in Americans of African, Hispanic, and Asian heritage. The highest incidence of all is among Native Americans.
- In 1997, the average cost of health care for each American with diabetes was over $10,000 per year, compared to approximately $2,500 per year for Americans without diabetes.
* retina is the back inner surface of the eyeball that plays a key role in vision. This surface contains millions of light-sensitive cells that change light into nerve signals that the brain can interpret.
How Can Diabetes Affect a Person's Life in the Future?
Both Type 1 and Type 2 diabetes can have negative long-term effects on a person's health. These effects tend to develop very slowly and gradually. Because a person with diabetes may not process fat properly, there tends to be damage to the blood vessels in the body, which increases the chances for high blood pressure, heart attacks, and strokes. Diabetes can also have long-term effects on the eyes, because tiny blood vessels in the retina * become weakened. If these blood vessels burst, they can cause bleeding and scarring in the eye, or even blindness. The chance of nerve damage, and of developing kidney disease, is also increased in a person with diabetes. Finally, foot health can become an issue for people with diabetes: because the condition can affect circulation to the feet, small cuts or wounds can turn into serious infections without proper care.
People with diabetes can take steps to help prevent or lessen the effects of these long-term problems. Recent research has shown that blood sugar control is a key factor. It is very important for people with diabetes to have regular physical checkups, when a doctor can monitor blood pressure and foot health, check fat levels in the blood, and look for problems with the kidneys. Annual trips to the eye doctor are crucial for people with diabetes. If the
ophthalmologist * discovers problems with the blood vessels in the retina, vision problems often can be prevented or lessened with
laser surgery.
While people with diabetes must depend on doctors and other medical professionals to help them, they can also do quite a bit to help themselves. Continued education about proper diabetes management is a key part of helping people with diabetes stay healthy.
Medic Alert Tags
People with diabetes often wear metal tags or bracelets imprinted or inscribed with important medical information. In the event of an accident or diabetic coma, the information on the tag can alert medical personnel about the patient's condition.
Some companies offer medical alert tags that have an identification number that is unique to the individual so that a doctor who doesn't know the person can retrieve the patient's medical history in the event of emergency.
* ophthalmologist is a medical doctor who specializes in treating diseases of the eye.
Banting, Best, and the Dog With Diabetes
Two scientists and a dog may sound like characters in a movie, but it was just such a threesome who were involved in discovering insulin. Shortly after World War I had ended, a Canadian surgeon named Frederick Banting (1891-1941) became very interested in diabetes and how the pancreas functions in a person with diabetes. A neighborhood child had died from diabetes, and this helped pique Banting's interest in making discoveries about the condition.
In his University of Toronto laboratory, assisted by a graduate student named Charles Best, Banting took out the pancreas glands of several dogs (which caused the dogs to develop diabetes), extracted their insulin, and began investigating the properties of insulin. Banting and Best discovered that insulin brought down the level of blood glucose in the dogs' blood; the dogs who had their pancreas glands removed could now survive, as long as they had insulin injections. A famous photo was taken of the two scientists in 1921, and between them stands the very first dog with diabetes that was kept alive with insulin.
In 1923, Sir Frederick Banting and the Scottish scientist John James Macleod (1876-1935) were awarded the Nobel Prize for medicine and physiology for their discovery of insulin.

Best, Banting, and one of the dogs they treated with insulin, April 1922.
Courtesy Banting House National Historic Site Collection.
Will There Ever Be a Cure?
Diabetes research is an active field. Much of the scientific work is concerned with insulin: how to get it into the body, or how to get the body to produce it on its own. Since insulin cannot be swallowed, researchers have been investigating other ways to get it into the bloodstream without an injection, such as eye drops, nasal sprays, and inhalers. They have also experimented with pancreas transplantation, as well as transplantation of the islet cells that make insulin. Until there is a cure for diabetes, however, people must live with it and control it using the information and equipment available to them now.
Greek Speak: A Diabetes
Dictionary
Many English words come from Greek. These include many of the words used to describe diabetes, as well as the word "diabetes" itself.
Diabetes Greek for "passing through," because Greek doctors noticed how much liquid people with diabetes drank, and how often they needed to urinate.
Mellitus Greek for "honey-like" or "sweet," because it was noticed that the urine of people with diabetes smelled sweet, due to its high sugar content.
Insulin Greek for "island." The groups of islet cells in the pancreas that are responsible for making insulin and other hormones look like tiny islands under a microscope.
Hypo Greek for "below," and thus "too little."
Hyper Greek for "above," and thus "too much."
Glyk Greek for "sugar."
Emia Greek for "blood."
ON HOW TO MONITOR BLOOD SUGAR LEVEL,KINDLY CLICK HERE.